First of all, it’s important to understand what diabetic foot is. Practically no “normal” person knows what it is, but everyone who has diabetes—or lives with someone who does—has, unfortunately, learned about it.
It is a very common and serious complication of diabetes, which must be carefully prevented and can now be treated by also considering aspects that until recently were little known—such as those related to glycation.
Diabetes complications are truly numerous, but while obesity, fatty liver, and cardiovascular diseases are often perceived by the patient as if they were “additional illnesses,” diabetic foot is something that causes pain, breaks the skin—often even affecting the flesh—generates a persistent foul odor, and is constantly felt as an irritating “thorn” that the person suffering from it carries with them every hour of the day. It is part of their body and makes its presence known, which explains the deep desire to ease its torment.
Diabetic foot is caused by years of uncontrolled hyperglycemia, which damages blood vessels and nerves. The deterioration of nerves and blood vessels actually begins many years before diabetes becomes clinically evident.
The new development today is that we can go beyond the traditional treatment of the condition (antibiotics, painkillers, antidiabetic drugs, etc.) thanks to a better understanding of how low-grade inflammation and glycation play a significant role in the onset of diabetic foot. By making targeted nutritional changes, it is now possible to influence many of the factors that keep the condition active and troublesome.
As mentioned, this is one of the most common chronic complications of diabetes mellitus. It involves a combination of peripheral neuropathy (nerve damage) and vasculopathy (microcirculation impairment), which reduce sensitivity, slow down healing, and increase the risk of infections. Without proper care, it can progress to ulcers and deep infections that, in the most severe cases, may lead to amputation of toes or even the foot.
Main Symptoms of Diabetic Foot
- Loss of sensitivity to touch, heat, or cold, along with unusual types of pain
- Tingling, burning sensations, or electric shock-like pains in the feet
- Minor infections around the edges of the nails
- Prolonged redness and areas of irritation on the foot’s skin
- Ulcers or small wounds that do not heal
- Dry, cracked skin or small cuts
- Abnormal coloration of the foot or toes
- Foot deformities (such as hammer toes or bunions)
- Persistent odor or signs of local infection
Diabetic foot is caused by years of uncontrolled hyperglycemia, which damages blood vessels and nerves. This damage—both to nerves and circulation—begins many years before diabetes becomes clinically evident.
Glycation levels, which can be assessed by measuring methylglyoxal (MGO) and glycated albumin, cause vascular dysfunction well before fasting blood glucose and HbA1c levels begin to rise. (Mukohda et al., J Pharmacol Sci. 2009;109:305–10, for MGO’s impact on vascular function; and Paudel YN et al., Cells. 2020, 9, 383; doi:10.3390/cells9020383, for MGO-induced nerve tissue damage.)
Risk Factors for Developing Diabetic Foot:
- Long-standing diabetes
- Poorly controlled blood glucose and HbA1c
- Presence of glycemic spikes (fructose-related) and high glycemic variability
- Smoking (which further impairs local circulation)
- High blood pressure and elevated cholesterol
- Elevated BAFF levels (high BAFF impairs wound healing and increases the risk of infection)
- Inappropriate footwear
- Poor foot and nail hygiene
- Previous episodes of ulcers or infections (which indicate an already weakened immune response)
- Poorly managed vitamin and mineral deficiencies
In Italy, there are centers of excellence dedicated to the treatment of diabetic foot that do outstanding work, though they generally adhere to the currently established standard therapeutic protocols.
However, recent scientific advances make it possible to take an important step beyond these standards—toward healing—through a more personalized approach to care.
Prevention
Preventing diabetic foot in individuals already diagnosed with diabetes is both possible and essential:
- Regularly monitor blood glucose levels and keep both HbA1c and glycated albumin under control
- Examine and wash your feet daily, drying them carefully
- Wear comfortable, well-fitting shoes with no internal seams
- Trim your toenails properly and regularly
- Have your feet checked periodically by a professional (podiatrist or doctor)
- Follow a personalized diet and maintain a regular physical activity plan
Even before a diabetes diagnosis—especially in cases of family predisposition—it’s crucial to understand and assess your metabolic tendencies. Measuring your MGO (methylglyoxal) and glycated albumin levels can help identify your personal risk path and enable you to take early, preventive action against sugar-related tissue damage that may already be developing.
Recommended Tests
To prevent and monitor the risk of diabetic foot, it’s essential to evaluate both metabolic and inflammatory components. Recommended tests include:
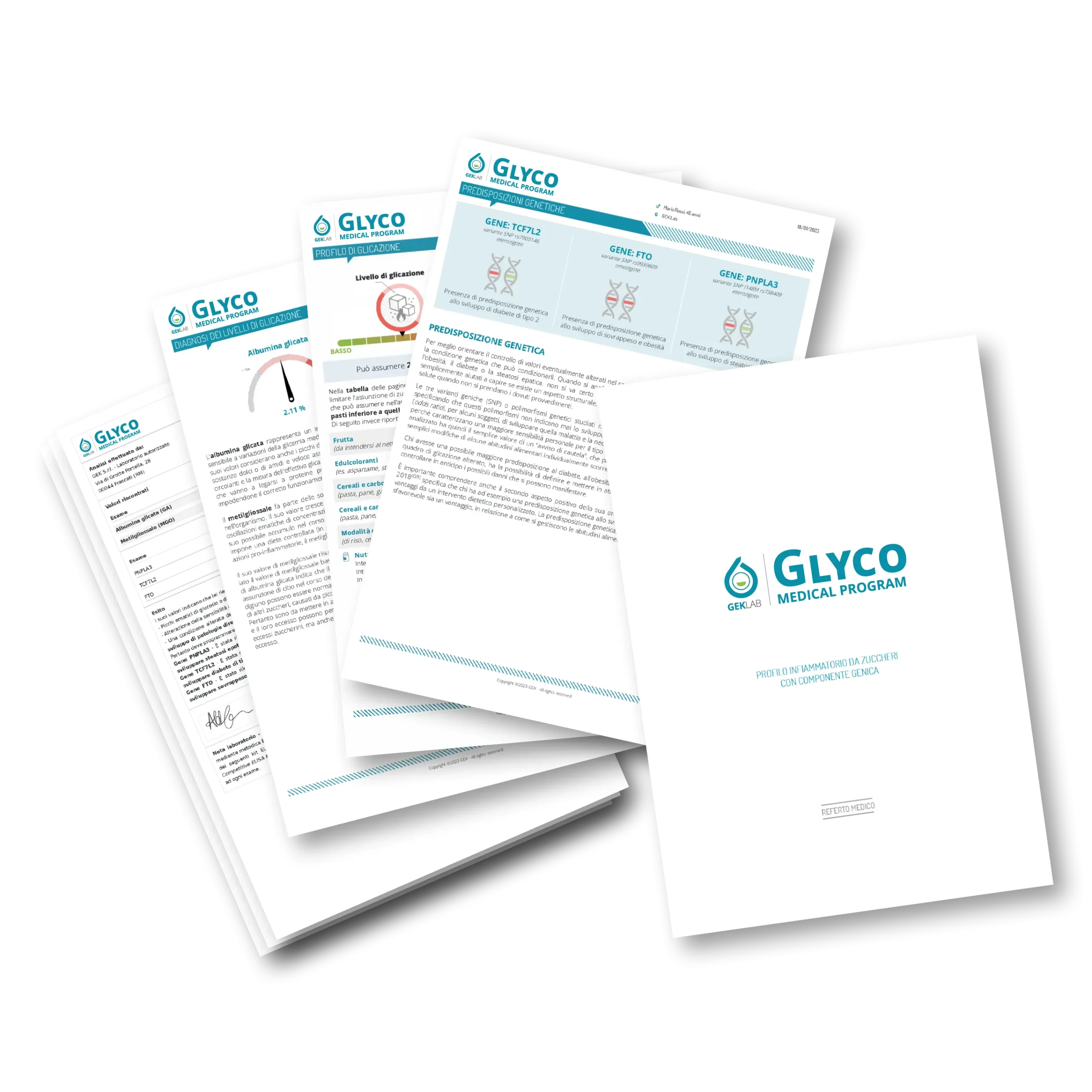
- Glyco Medical Program, an innovative test that measures glycation levels through glycated albumin and methylglyoxal (MGO).
- Usefull during the preventive phase, to detect silent glycemic stress
- Also essential for those who have already developed diabetic foot, as it helps monitor the effectiveness of nutritional and therapeutic plans, enabling personalized adjustments over time and supporting therapies aimed at controlling neurovascular damage
- Fundus examination and neurological screening – to assess diabetic neuropathy
- Lower limb color Doppler ultrasound – to evaluate microcirculation status and peripheral oxygenation
Conclusion
Diabetic foot can be effectively managed through a combination of prevention, clinical monitoring, and daily care.
Thanks to tools like the Glyco Medical Program, it is now possible to measure the real metabolic impact of sugars well before tissue damage appears, and to assess the effectiveness of dietary plans, supplements, and therapies over time. Monitoring MGO and glycated albumin levels helps track patient adherence and adjust interventions accordingly. Don’t wait for symptoms to appear—early action is the real cure.
Edited by The Scientific Editorial Team GEK Lab