Crohn’s Disease (formerly known as Morbus Crohn) is a chronic inflammatory bowel disease (IBD) that can affect the entire gastrointestinal tract, with a preference for the final sections of the intestine—namely, the ileum and colon. The main symptoms of Crohn’s include abdominal pain, persistent diarrhea, fatigue, weight loss, and often malabsorption and extraintestinal complications. But what is really happening inside the body of someone affected by Crohn’s? And more importantly, how can we approach Crohn’s disease not only with medication, but also by thoroughly assessing the contributing factors behind the condition—taking into account aspects such as diet, inflammation, and glycation?
Crohn’s: An Immune and Inflammatory Response Also Linked to Diet
Crohn‘s disease is often treated with immunosuppressive or biological drugs, which are essential for controlling the acute phase and are carefully selected to help prevent relapses over time.
Studies and clinical observations show that repetitive or excessive consumption of certain foods (which vary depending on dietary habits) is strongly correlated with the onset of the disease and can individually worsen the symptoms of Crohn’s, especially in individuals with intestinal dysbiosis or an altered mucosal barrier.
However, it is important to understand that chronic inflammation in Crohn’s disease is often a defensive response, and not necessarily a malfunction of the immune system.
In fact, the body can activate persistent inflammation in response to repetitive or excessive dietary stimuli, such as those caused by a diet rich in industrial and ultra-processed foods, simple sugars, or the repeated use of certain foods (such as wheat and dairy in Europe, or rice and soy in the East).
In this scenario, Crohn’s disease represents an important warning sign, indicating an imbalance at the intestinal, immune, and metabolic levels.
The Role of Diet in Crohn’s Disease
One of the most discussed aspects in managing Crohn’s disease is the role of diet. Studies and clinical observations show that repetitive or excessive consumption of certain foods (which vary depending on dietary habits) is strongly correlated with the onset of the disease and can individually worsen the symptoms of Crohn’s, especially in individuals with intestinal dysbiosis or an altered mucosal barrier. This is because the repeated intake of certain foods leads to the development of persistent, low-grade inflammation, which predisposes to the onset of the disease and the worsening of symptoms.
This is not about demonizing certain foods outright, but rather about modulating the food load based on the individual’s dietary profile. In many cases, the issue is not the single food, but its repeated consumption in an already inflamed body.
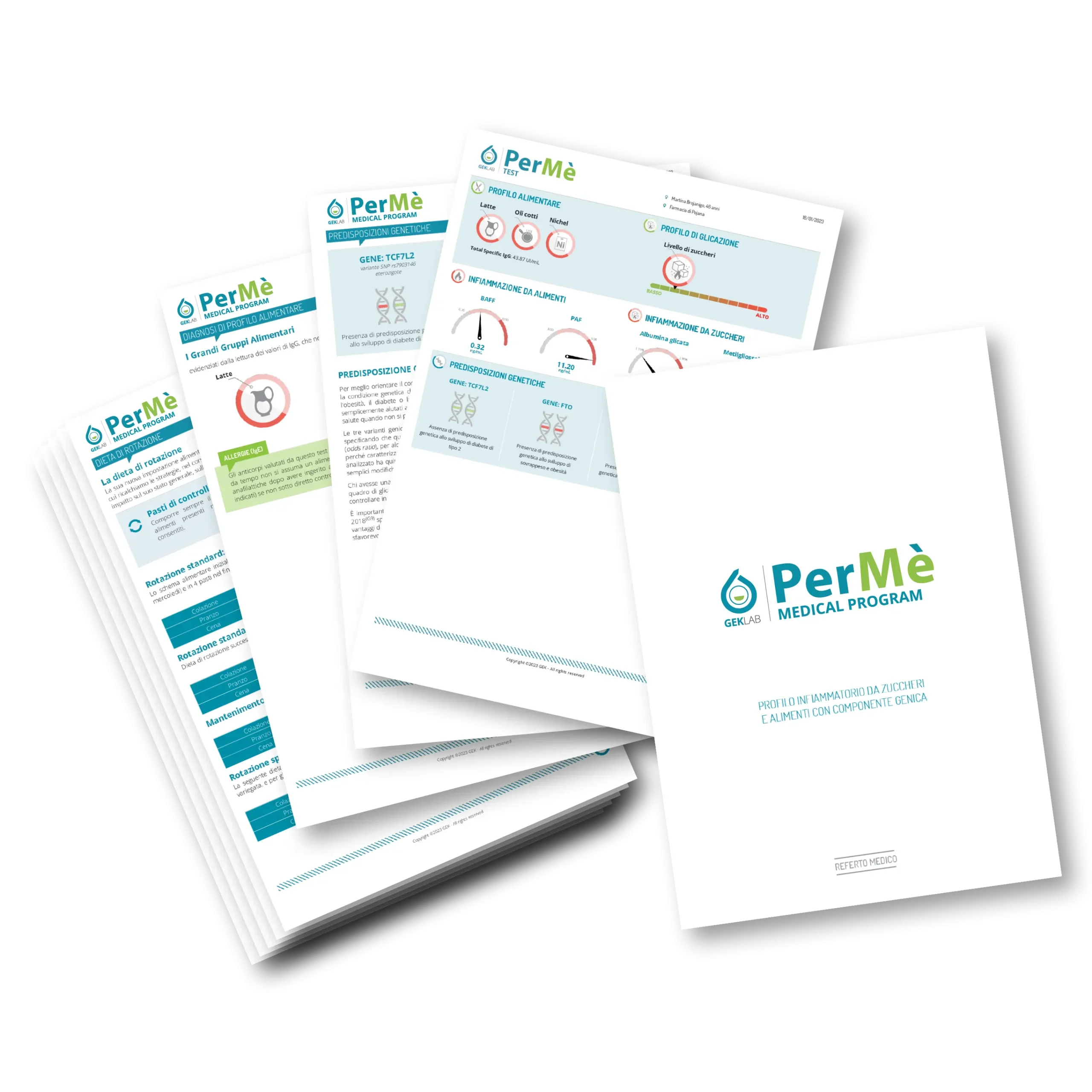
The individual dietary profile, which signals the level of food-induced inflammation in the body and precisely identifies which food groups are being overconsumed, is assessed through the Recaller Medical Program and the PerMé Medical Program.
Based on the results obtained, personalized nutritional suggestions can be made to significantly reduce intestinal inflammatory aspects.
The inflammation caused by the repetitive use of certain foods (always defined on an individual basis) and the effects of glycation (related to the intake of sugars and assimilable substances) also lead to alterations in the microbiota, which are themselves pro-inflammatory. This means that if glycation and inflammation are not controlled, support with pre- or post-biotics may not have a therapeutic effect.
Crohn’s Disease and Glycation: An Often Overlooked Connection
A lesser-known but crucial aspect in managing Crohn’s disease is glycation. This process occurs when excess sugars bind to proteins, enzymes, DNA, and lipids, forming what are known as AGEs (Advanced Glycation Endproducts). These molecules promote inflammation, oxidative stress, and tissue damage, worsening the already fragile condition of the intestinal mucosa in Crohn’s patients.
A glycated organism is more reactive, less resilient, and more prone to developing or intensifying the symptoms of Crohn’s disease. Glycation can act as a silent aggravating factor, responsible for unexplained clinical worsening even during periods that seem stable.
Managing Crohn’s Disease: An Integrated Approach
Managing Crohn’s disease cannot be limited to just suppressing inflammation with medication. It is essential to develop a systemic approach that includes dietary modulation, support for the intestinal microbiota, control of glycation, and an objective assessment of the inflammatory load.
From a nutritional standpoint, a low glycemic load and anti-inflammatory diet, with rotational respect for the foods highlighted by one’s individual dietary profile, can help reduce the underlying inflammatory noise. Targeted supplements with glutamine, zinc, vitamin D, polyphenols, and selected probiotics can strengthen the intestinal barrier and improve immune resilience.
A distinctive element is the use of the Glyco Medical Program by GEK Lab, an innovative diagnostic protocol that allows for the objective measurement of systemic glycation levels and the identification of any latent inflammatory state. This information enables the physician to personalize the intervention based on concrete data, improving the effectiveness of nutritional and integrative strategies for patients with Crohn’s disease.
Conclusion: Listen to Crohn’s, Not Just Treat It
Crohn’s disease is not just an illness to be contained, but also a warning signal from the body that must be properly interpreted. It is a reflection of an imbalanced system that reacts to an often underestimated inflammatory load. Addressing food-related inflammation—by reducing glycation, dysbiosis, food overload, and oxidative stress—means supporting the body in healing or at least improving clinically, alleviating symptoms, and reducing the need for aggressive interventions. This approach helps control the disease and promotes a more stable and lasting remission.
Edited by The scientific Editorial Team GEK Lab